While LASIK remains the procedure of choice for most refractive surgeons
in the treatment of mild to moderate myopia, new types of surface ablations
are gaining popularity as an option for a cross-section of patients who
are unsuitable candidates for such procedures. At a EuroTimes Educational
Satellite Symposium held at the XXIII Congress of the ESCRS Lisbon, speakers
explored the potential advantages of the new surface ablation procedure
Epi- LASIK performed with the Moria Epi-KTM epithelial separator.
 Alaa El-Danasoury, FRCS Medical Director Chief, Refractive Surgery Service
Magrabi Hospitals & Centers malaa@magrabi.com.sa
Alaa El-Danasoury, FRCS Medical Director Chief, Refractive Surgery Service
Magrabi Hospitals & Centers malaa@magrabi.com.sa
Jorge L. Alio MD PhD Professor and Chairman of Ophthalmology VISSUM, Instituto
Oftalmologico de Alicante Universidad Miguel Hernandez, Alicante, Spain
jlalio@vissum.com
Dr Alaa El-Danasoury told the symposium that LASIK is likely to remain
the preferred option for patients who are suitable for such procedures
because it involves less pain provides more rapid visual recovery and
entails no risk of haze. However, there are patients with low to moderate
refractive errors who are unsuitable for LASIK but who may nonetheless
be suitable for surface procedures. They include patients with relatively
thin corneas and those who are extremely cautious about ocular surgery
involving separators.
New surface ablation techniques
A number of new variations on conventional PRK have been developed over
recent years to address the needs of such patients.They include LASEK,
the application of mitomycin-C and, more recently, Epi-LASIK. Each of
the techniques aims to reduce postoperative pain, speed visual recovery
and above all, eliminate haze.There remains some controversy, however,
regarding both their superiority in terms of safety and efficacy compared
with conventional PRK.
In the case of LASEK, there have been conflicting reports regarding reduced
pain and haze with the procedure.The LASEK technique involves loosening
and lifting the epithelium with alcohol and replacing it after the ablation.The
theory is that the epithelium will remain viable and therefore not stimulate
a healing response in the keratocytes in the underlying stroma. However,
it has been demonstrated that the alcohol used in the procedure actually
kills the epithelial cells. It is therefore debatable whether the epithelial
flap actually confers any benefits.
Mitomycin-C is used in surface ablation procedures as a means of preventing
haze by dampening down the keratocyte response to the ablation. But the
agent is extremely toxic, and its longterm effects on the keratocytes
and the corneal collagen remains unknown.
“This is an area of controversy, it is unknown when the cornea will recover
its normal immune physiology and there are no longterm studies on the
effect of mitomycin on the cornea. I am reluctant to kill the stromal
keratocytes because these patients have to live the rest of their lives
with a good corneal immunity.”
Epi-LASIK flaps more viable
The newest of the techniques Epi-LASIK is free of the many of the drawbacks
of the older surface ablation techniques. The procedure involves the mechanical
separation of the epithelium from the stroma with a specially designed
device. It therefore involves no toxic substances. Moreover, the technique
separates the epithelial sheet below the lamina densa. Research has shown
that the epithelial tissues in the separated flap remain viable in 85%
of cases (Pallikaris et al, JCRS, August, 2003).
Dr El-Danasoury noted that a surface ablation procedure that does not
cause haze would be of particular value in the treatment of patients who
are more prone to haze, such as brown-eyed Middle-Eastern individuals.
“In the Middle East we do not perform many PRKs because of the higher
risk of haze.We’ve seen haze for very low myopia, as low as two or three
dioptres. But there are many patients who are not good candidates for
LASIK and surface ablations would be a good choice for them if we could
do it without inducing haze.”
The Moria Epi-K epithelial separator
Surgeons now have at their disposal a new system that fully automates
the creation of epithelial flaps in the form of the Moria Epi-KTM.The
new device consists of a special lightweight handpiece and a disposable
head.
 The
Epi-K’s handpiece has two motors, one for head advancement and the other
for oscillation of the separator.The advancement speed is specifically
calibrated for epithelial separation. The
Epi-K’s handpiece has two motors, one for head advancement and the other
for oscillation of the separator.The advancement speed is specifically
calibrated for epithelial separation.
The disposable head encases a pre-assembled non-cutting separator.The
angle of the separator to the epithelium allows for cleavage of the epithelial
layer while an applanation front plate prevents the instrument from cutting
into the stroma.
“The Epi-K really does what it says, we have used the device in 60-65
patients and we have not really had any problems so I am confident that
the machine is very precise.”
Epi-LASIK in haze-prone eyes
He added that in a comparative study he recently carried out involving
haze prone eyes, PRKtreated eyes had significantly more haze than eyes
that underwent Epi-LASIK with Moria Epi-K. In fact, the Epi- LASIK-treated
eyes were virtually haze-free in all cases.
The prospective bilateral randomised clinical trial study involved 26
eyes of 22 Middle- Eastern brown-eyed patients who underwent Epi-LASIK
with the Epi-K device.A subgroup of 15 consecutive patients underwent
Epi-LASIK in one eye and PRK in the other.
The patients in the study had a mean age of 22.3 years (range: 9-33 yrs).
All were unsuitable for LASIK because of thin corneas. Their mean preoperative
spherical equivalent was-2.90 D (range: -4.75D to -1.13 D). Patients were
excluded from the treatment if they were keratoconus suspects, had dry
eyes, unstable refraction, or had undergone previous ocular surgery.
Epi-LASIK technique
Dr El-Danasoury commences his Epi-LASIK procedures by first applying topical
anaesthesia.After putting on the suction ring he then assembled the device
on the eye and used the slow speed of the Epi-K device to move it forward
across the eye.
“The eye should be continually moistened throughout the procedure to avoid
tearing the epithelial tissues. Once you reach the hinge site you reverse
the motor and it goes backwards. It is really simple and easy to use,”
Dr El-Danasoury noted.
When he has created the flap he uses balanced salt solution to move it
out of the way during the ablation. Following the ablation he manipulates
the flap back into place with a salinesoaked sponge. He then applies hypertonic
saline to make the epithelial flap more adherent. He then applies antibiotic
drops and places a bandage contact lens on the eye.
Operative complications in his study included a total flap cut in one
eye, which subsequently underwent conventional PRK and was excluded from
the study results. In another eye a stromal injury occurred when the epithelial
separator hit a metallic instrument.Although the eye had a good visual
outcome, Dr El- Danasoury said he now preassembles the Epi-K instrument
before applying it on the eye to avoid such complications.
Similar efficacy and predictability
The uncorrected visual acuity results at two months were very similar
in the two treatment groups. In the Epi-LASIK group, 73% achieved 20/20
or better, 93% achieved 20/25 or better, and 91% achieved 20/30 or better.
In the PRK group, 71% achieved 20/20 or better, 86% achieved 20/25 or
better, and 93% achieved 20/30 or better. All eyes were 20/40 or better
at three months.
The Epi-LASIK treated eyes appeared to fare slightly better than the PRK-treated
eyes in terms of BCVA, although the difference did not reach statistical
significance. Half of the eyes in the Epi-LASIK group gained one or two
lines, compared to 43% in the PRK group, while 5.0% of the Epi- LASIK
group and 7.0% in the PRK group lost one line of BCVA. No eyes in either
group lost two or more lines of BCVA. Visual rehabilitation appeared to
be more rapid in the Epi- LASIK treated eyes. At the fourth postoperative
day, 50% said they saw better in their Epi-LASIK eye, while only 16.7%
said they could see better in their PRK eye.
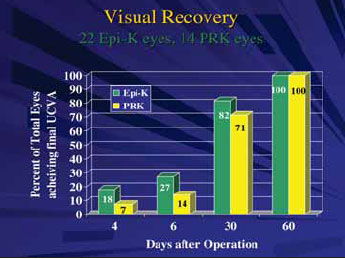
In addition, 18% had achieved their final refraction by day four in the
Epi-LASIK group, compared to only 7% of eyes in the PRK group. By day
seven 27% had achieved their final refraction in the Epi-LASIK group,
compared to only 14% in the PRK group. However by two months all eyes
in both groups had achieved their final refraction.
The two groups had similar results in terms of postoperative pain. On
the first postoperative day, four patients (28.6%) reported less pain
in the Epi- LASIK treated eye and six (42%) reported less pain in the
PRKtreated eye and the remaining patients reported no difference between
their two eyes. By the second day six (54.5%) reported less pain in their
Epi-K eye and two (18.2%) reported less pain in PRK eye. By the fourth
day all patients said they were virtually pain-free in both eyes.
“There was not much difference between the two groups in the pain they
experienced.The first couple of days patients reported pain in both eyes
but by the fourth day they were almost free of pain.”
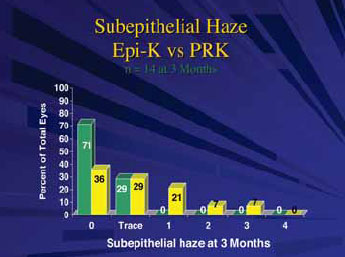
Significantly less haze
Dr El-Danasoury noted that the most important difference between the two
groups was in the occurrence of subepithelial haze. At three months postoperative,
in the Epi-LASIK eyes there was a trace of haze in 29% and the remaining
eyes remained totally clear at three months. By comparison, in the PRK-treated
eyes 29% had a trace of haze, 21 % had level one haze, seven percent had
level 2 and a further 7% had level 3 haze.
In summary, Dr El-Danasoury said that the Epi-K epithelial separator is
effective in creating epithelial flaps and that there is less risk of
haze with Epi-LASIK compared with PRK.The technique also has efficacy
and predictability similar to PRK but has a relatively faster, less painful
visual recovery. “I think now we have a good alternative for many patients
who are not good candidates for LASIK and do it without the need to place
toxic substances on the cornea and if we can do it without haze then this
represents a step forward.”
Epi-LASIK and corneal biomechanics
 While LASIK does not entail the risk of haze, it may be less predictable
than surface ablation procedures because of the effects of flap creation
on corneal biomechanics, Prof. Jorge L.Alio MD PhD told the symposium.
The degree to which flap creation alters the biomechanics
While LASIK does not entail the risk of haze, it may be less predictable
than surface ablation procedures because of the effects of flap creation
on corneal biomechanics, Prof. Jorge L.Alio MD PhD told the symposium.
The degree to which flap creation alters the biomechanics
of the cornea depends on a range of factors.They include the size, thickness
and regularity of the flap, the size, flap centration and position of
the hinge, and the curvature of the interface. Postoperative factors also
come into play including corneal wound healing and interface reactions.
The result of all these factors is that the postoperative radius of corneal
curvature will be at variance from what was intended. As a consequence
eyes can be over- or under-corrected and customised ablations will lose
some of their precision.
Comparative studies shows least change in corneal biomechanics
with Epi-LASIK
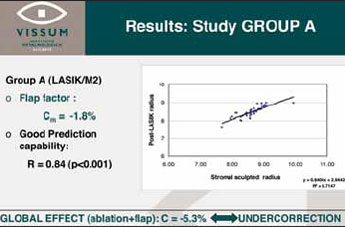
Dr Alio told the symposium that in a comparative study he conducted
involving 81 eyes of 81 patients, in those treated with Epi- LASIK there
was only a negligible difference between the intended postoperative radius
of curvature and that which was intended, while there were significant
differences between the intended and achieved corneal curvatures in eyes
treated with LASIK or LASEK.
The patients in the study had myopia or myopic astigmatism and a preoperative
spherical equivalent ranging from–2.0 D and –8.0 D. They ranged in age
between 22 and 57 years. Dr Alio randomised his patients into three treatment
groups. In the first group, 40 patients underwent LASIK with flaps created
with a Moria M2 microkeratome. In the second group, 21 patients underwent
LASEK, and in the third group 20 patients underwent Epi-LASIK with the
Moria Epi-K epithelial separator. In all eyes, Dr Alio performed the ablations
with the Esiris excimer laser (Schwind) using the same standard algorithm.
Coefficient of biomechanical response
At one months’ follow-up Dr Alio used topography to determine the effect
of corneal biomechanics on the resulting corneal curvature. He obtained
a coefficient of the biomechanical response by dividing the difference
between the post surgical corneal radius of curvature and the calculated
sculpted curvature radius by the calculated sculpted radius of curvature.
“The coefficient characterises the change in corneal curvature due to
such factors as flap relocation and the ablation profile by excimer laser.
Therefore, if it is greater than zero it means the cornea has been excessively
flattened, that, for myopic correction, is overcorrected. If on the other
hand, the value is less than zero it means the cornea remains steeper
than planned, or undercorrected,” Dr Alio explained.
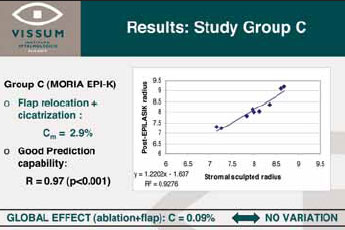
The results showed that in the Epi-LASIK group the coefficient of variation
between the precalculated sculpted radius and the postoperative radius
was minimal (mean:0.09%). By comparison, the coefficient of the biomechanical
response was –5.3% in the LASIK group and –2.3% in the LASEK group, indicating
significant undercorrection. Correspondingly, the predictability of the
procedure was higher in the Epi-LASIK group (0.97) than in the LASIK group
(0.84) or the LASEK group (0.71).The superior predictability of the results
in terms of topography was also reflected in the patients’ refractive
outcomes he noted.
Different results with different surface ablation techniques
Dr Alio noted that the better predictability of Epi-LASIK compared with
LASEK came as somewhat of a surprise. “We had thought that Epi- LASIK
and LASEK were equivalent procedures in terms of the effect they have
on biomechanical changes of the cornea, but our results indicate that
they are not. It may be that the epithelial toxicity in LASEK plays a
role that is not present in Epi-LASIK or that the smoother surface to
be ablated preserves the corneal biomechanics.”
In conclusion, Dr Alio said that Epi-LASIK caused the least biomechanical
change of the three techniques in the study. He suggested furthermore
that an increase in the quality of excimer laser outcomes might be expected
with Moria Epi-K epithelial separator.
“It is in the periphery of the ablation that most of the biomechanical
changes of the cornea following corneal refractive procedures occur and
the more we are able to control those changes, the more the quality of
vision results will improve in our patients,” he added.
|
 Список
статей
Список
статей
 Список
статей
Список
статей