Страничка клинициста
Treatment of Retinal Breaks with Large-Spot Diode Laser Photocoagulation
 Список
статей Список
статей |
|
| Saurabh Jain, MS, MRCOphth R. S. B. Newsom, FRCOphth,
MD J. D. A. McHugh, MD, FRCS, FRCOphth |
|
| Abstract. A
new technique is described for treating peripheral retinal breaks using
large-spot, diode laser retinopexy. A large-spot (1.2 to 3.0 mm) diode laser
(810 nm) was used to treat patients with breaks in attached retina. Powers
between 800 and 1,200 mW produced a uniform retinal photocoagulation beyond
the break margins. Patients were observed monthly until an adequate chorioretinal
scar had formed. Eleven eyes were treated using this technique. Satisfactory
retinopexy was obtained in all cases. The effi ciency of large-spot diode
laser photocoagulation for retinal breaks and its advantages over conventional
laser and cryopexy techniques justifi es further studies into this technique.
[Ophthalmic Surg Lasers Imaging 2005;36:514-517.] INTRODUCTION Laser retinopexy is an effective treatment for peripheral retinal breaks.1-6 It produces strong chorioretinal adhesion with little blood–retinal barrier disruption and few macular complications.5,6 As an alternative to argon (λ 514 nm) and frequency-doubled YAG (λ 532 nm) lasers, the diode laser (λ 810 nm) using a small spot size (100 to 500 µm) has been widely used for photocoagulation, particularly in patients with retinopathy of prematurity, and diabetic retinopathy.7,8 Photocoagulation using large-spot diode lasers (800 to 5,000 µm) has been employed for the treatment of choroidal melanomas9,10 and with subthreshold power for choroidal neovascular membranes. 11-14 We describe a new technique for treating peripheral retinal breaks using large-spot laser photocoagulation and we evaluate the effi cacy and safety of this technique. TECHNIQUE Patients with symptomatic retinal breaks were recruited from the Kings College Hospital Retinal Service. Pretreatment investigations included Snellen visual acuity, anterior segment slit-lamp examination, tonometry and dilated funduscopy with a Goldmann 3 mirror lens, and indirect ophthalmoscopy with indentation. Eyes with retinal tears or holes with posterior vitreous detachment were included. Informed consent was obtained from patients before inclusion. The type, location, and size of the tear were noted along with the presence of hemorrhage. Provided the anterior edge of the break could be visualized at the slit lamp, the patient was recruited for the trial. 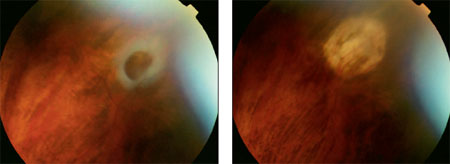 Figure
1. Fresh retinal break in the periphery following spontaneous posterior
vitreous detachment. Figure
1. Fresh retinal break in the periphery following spontaneous posterior
vitreous detachment.Figure 2. Appearance of the tear 1 year after laser treatment demonstrating a well-established chorioretinal scar. A slit-lamp mounted diode laser (IRIDEX Corporation, Mountain View, CA) was used with a spot size between 800 and 3,000 µm. Eyes were anesthetized with benoxinate hydrochloride 0.4% (Chauvin Pharmaceutical Ltd., Essex, United Kingdom) and a Volk Superquad XL wide-fi eld contact lens (Volk Optical Inc., Mentor, OH) was used to focus the laser on the retina. The spot size was adjusted to overlap the margins of the break to approximately 200 µm. A long pulse exposure (10 seconds) was selected with a power suffi cient to produce a uniform whitening reaction. The treatment parameters of power, exposure time, and number of pulses were recorded for each patient. Threshold energy was determined principally by duration of exposure, after setting the treatment power. The latter was estimated on the basis of retinal pigment epithelial pigmentation and selected spot size. Typical parameters employed were power between 800 and 1,200 mW, spot size of 1.2 to 3.0 mm, and pulse duration of 5 to 10 seconds. Patients were observed monthly until an adequate chorioretinal scar had formed around the treated break. The follow-up period ranged from 3 to 18 months to evaluate the long-term changes in the treated eyes. The local ethical committee supervised this pilot study. Sample Case. A 52-year-old white woman was found to have a retinal tear in the temporal retina of her left eye following a spontaneous posterior vitreous detachment (Fig. 1). She underwent diode laser retinopexy (power = 1,500 mW; spot size = 3 mm; pulse duration = 8 seconds) to seal the hole. Following treatment, a satisfactory chorioretinal adhesion developed, which was stable at 1 year (Fig. 2). Eleven eyes of 11 patients were treated using this technique with a minimum review period of 6 months. In all cases, satisfactory reactions were obtained. At 6-week review, all breaks were closed (Figs. 1 and 2). The laser-treated area in all cases exhibited a marked chorioretinal scar surrounding the retinal breaks. No complications occurred during or after the laser retinopexy and no corneal, iris, or lenticular burns were noted. Two patients reported mild discomfort during the procedure, probably attributable to the fact that the break was located in the region of a ciliary nerve, but they did not require retrobulbar or peribulbar anesthetic; no late scar retraction occurred. This method has now become the technique of choice for treating retinal breaks at our center. DISCUSSION Previous researchers have studied the use of diode laser to stimulate chorioretinal adhesion in primate eyes.15-29 The greater penetration of the infrared emission formed deeper chorioretinal scars than those generated with shorter wavelengths, with the potential for greater mechanical adhesive strength. Isola et al.30 described diode laser transpupillary retinopexy, using 3 to 5 rows of 500-µm contiguous laser spots around the retinal lesion. They found that diode laser therapy was effective at creating a satisfactory chorioretinal adhesion, but noted diffi culty in creating scars in hypopigmented fundi. We describe a novel method of treating retinal breaks that is effective at inducing a satisfactory chorioretinal scar. In contrast to Isola et al.’s study, we used a confl uent laser spot to completely cover the retinal beak and observed consistent and satisfactory chorioretinal scars irrespective of the amount of pigmentation. Cryotherapy for larger breaks requires local anesthesia, and may cause postoperative infl ammation, retinal pigment epithelial dispersion, and blood–retinal barrier breakdown, increasing the risk of proliferative vitreoretinopathy and epiretinal membrane formation. In conventional laser therapy, a double or triple row of burns is applied around the lesion. This is not only more time-consuming, but it is often diffi cult to obtain a confl uent reaction and therefore produce a homogeneous fi broglial scar.3 By contrast, large spot exposures enable a uniform whitening to be obtained across the break and extending onto normal retina in a few seconds. It also has the advantage of better transmission of the infrared light to the retina through lenticular opacities and vitreous hemorrhage and may also cause less retinal pigment epithelial cellular dispersion. The proven effi ciency of large-spot diode laser photocoagulation for retinal breaks justifi es further exploration of the potential of this novel technique, for both breaks and retinal degeneration. |
|
REFERENCES |
|
 |
|



